October 2024
Managing Bursitis in the Heel

Heel bursitis occurs when the bursa, a small fluid-filled sac, becomes inflamed. It is a common injury in athletes, active people, and people who stand for long periods of time.The bursa serves as a cushion between the heel bone and surrounding tissues, helping reduce friction and pressure. Bursitis in the heel often leads to throbbing heel pain, especially when walking or running, and can make even simple daily activities uncomfortable. Pain is usually most noticeable when the heel first strikes the ground, and the area may appear swollen or feel warm to the touch. A podiatrist can identify the best treatment approach to alleviate discomfort from heel bursitis. Common strategies include recommending footwear modifications, such as using cushioned shoes, or prescribing orthotic inserts to reduce pressure on the heel. This foot doctor also may administer corticosteroid injections to reduce inflammation. If you are experiencing heel pain, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis and treatment.
Many people suffer from bouts of heel pain. For more information, contact Dr. Scott Shrem of Garden State Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes of Big Toe Pain

Big toe pain can result from biomechanical problems or arthritis in the metatarsophalangeal, or MTP joint, where the base of the toe meets the foot. Biomechanical issues arise when there is an imbalance in the way the bones, tendons, and muscles function together, causing pressure to shift to the front of the foot. This action can lead to bunions, where the big toe pushes against the second toe, and turf toe, caused by overextending the toe during high-impact activities. Arthritis-related pain is the result of joint inflammation from gout, osteoarthritis, or rheumatoid arthritis. Symptoms often include swelling, stiffness, and difficulty walking. A podiatrist can help by diagnosing the underlying cause of the big toe pain. Treatments like custom orthotics, specific exercises, or in some cases, surgery may be suggested. If you are experiencing pain in the big toe, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact Dr. Scott Shrem of Garden State Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Key Facts About Morton's Neuroma
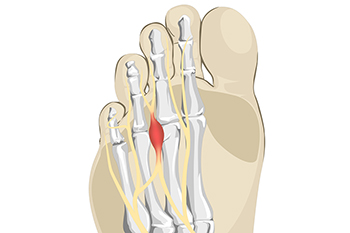
Morton's neuroma is a painful condition affecting the ball of the foot, typically between the third and fourth toes. It occurs when the tissue surrounding a nerve becomes thickened, often due to repetitive pressure or irritation. Common symptoms include sharp, burning pain in the affected area, tingling, or numbness that may radiate to the toes. Several risk factors contribute to the development of Morton's neuroma, including wearing tight or high-heeled shoes, engaging in high-impact activities, and having foot deformities like flat feet or bunions. Diagnosis usually involves a physical examination where a podiatrist assesses the foot's structure and evaluates symptoms. In some cases, imaging tests such as ultrasounds or MRI scans may be used to confirm the diagnosis. If you have pain in this part of your foot, it is suggested that you consult a podiatrist who can effectively treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Scott Shrem of Garden State Foot & Ankle Center. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Warts Can Be Treated!
Determining a Need for Orthotics

Determining if orthotics can help you often starts by evaluating signs of imbalance or improper foot mechanics. If your shoes wear unevenly, typically on one side, it can indicate poor alignment or overpronation, both of which orthotics can address. Frequent ankle sprains suggest instability that orthotics can help stabilize. Chronic foot, heel, knee, or low back pain may stem from improper foot function, and custom orthotics can provide support and improve alignment, relieving pressure on joints. If your toes are not straight or your feet point excessively inward or outward, orthotics may correct these issues by guiding your feet into proper alignment. If you think you might benefit from orthotics, it is suggested that you visit a podiatrist for an evaluation, foot and gait analysis, and determination if orthotics are right for you.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Scott Shrem from Garden State Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain May Indicate Plantar Fasciitis

Plantar fasciitis is a common condition that results in pain and inflammation in the heel and bottom of the foot. The primary symptom is a sharp, stabbing pain, particularly noticeable with the first steps in the morning or after prolonged periods of sitting. The discomfort often eases with movement but may return after long periods of standing or walking. This condition is typically caused by excessive strain on the plantar fascia, the thick band of tissue running along the bottom of the foot. Contributing factors include overuse, footwear that lacks ample cushioning, and having poor foot biomechanics, such as flat feet or high arches. Activities that involve repetitive stress, like running or standing for long periods, can also increase the risk. If you have heel pain, it is suggested that you visit a podiatrist who can offer an accurate diagnosis and treatment.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Scott Shrem from Garden State Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018