September 2024
Can Wearing High Heels Alter Foot Structure?

Wearing high heels can significantly impact the structure of your feet over time. These stylish shoes force the foot into an unnatural position, with the heel elevated and the toes pointed downward. This altered stance places excessive pressure on the forefoot, potentially leading to structural changes such as bunions, hammertoes, and increased risk of arthritis. The continuous use of high heels can shorten the Achilles tendon and weaken the calf muscles, affecting overall foot alignment and posture. Additionally, the lack of proper arch support in high heels can contribute to conditions like plantar fasciitis. If you have developed a foot condition from wearing high heels, it is suggested that you consult a podiatrist who can help you with an effective treatment plan.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Dr. Scott Shrem from Garden State Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Why High Heels Are Not Ideal for Healthy Feet
It is no secret that high heels are uncomfortable to wear for long periods of time. Although beauty is pain, you should not sacrifice the health of your feet for a stylish heel. Wearing high heels can potentially cause many different foot conditions that may be avoided by wearing proper footwear.
The structure of high heels forces weight of your body to get shifted forward toward the ball of the foot. The higher the heel you wear, the more weight and pressure get shifted forward. The pressure that your toes may experience from wearing heels may lead to hammer toes, bunions, and ingrown toenails. Extra weight and pressure resulting from wearing heels may cause stress fractures. Furthermore, heels may cause pinched nerves which may result in Morton’s neuroma.
High heels are even more dangerous for people who are clumsy. Falling or tripping while wearing heels can cause an ankle sprain or twist.
What many people don’t know is that heels can also cause back and knee problems. In order for your body to stay balanced on heels, your spine has to sway unnaturally, which adds stress to your spine muscles. This may cause you to experience a sore lower back.
If you decide to wear high heels regardless of the risks associated with them, there are ways you can minimize their harmful effects. One way to reduce injury is to massage and stretch your legs at the end of the day. Stretching can prevent the Achilles tendons and calf muscles from becoming too tight. If you are simply looking for more height, wedges and platforms provide a better surface area to distribute the body weight across compared to thinner heels.
If you experience pain from wearing high heels, it is important to see a podiatrist before any of your symptoms become worse.
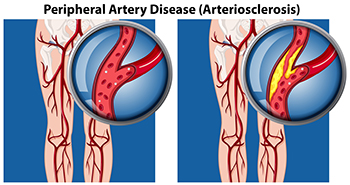
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Finding Relief for Peripheral Artery Disease in the Feet
Peripheral artery disease, or PAD, affects blood flow to the extremities, often causing pain, numbness, and discomfort in the feet. To find relief from PAD, managing underlying conditions like diabetes and high blood pressure is essential. Regular exercise, such as walking, can improve circulation and reduce symptoms by encouraging blood flow. Wearing well-fitting, comfortable shoes helps alleviate pressure points and prevent sores. Maintaining a healthy diet and quitting smoking can also significantly benefit vascular health. In more severe cases, medical interventions like angioplasty or surgery might be necessary to restore blood flow. If you have this condition, it is suggested that you are under the care of a podiatrist who can perform regular foot health checks.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Scott Shrem from Garden State Foot & Ankle Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Arthritis Can Cause Pain in the Feet and Ankles
Symptoms and Treatment of Plantar Warts

Plantar warts, caused by the human papillomavirus, or HPV, often develop on the soles of the feet, leading to discomfort, especially while walking. Highly contagious plantar warts typically appear as firm, rough, and flat lesions, often with small black dots at the center. They commonly affect people who use communal showers, pools, or changing areas. While plantar warts can affect anyone, people with a weakened immune system are particularly vulnerable. Diagnosis of plantar warts is generally made through visual examination to differentiate the wart from similar skin conditions, like corns or calluses. Treatment provided by a podiatrist may include cryotherapy, where the wart is frozen off, or the application of topical salicylic acid to dissolve the wart over time. A podiatrist can also offer more advanced options if the wart resists initial treatment. If you have developed a plantar wart, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Scott Shrem from Garden State Foot & Ankle Center. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Puncture Wounds on the Foot

Puncture wounds on the foot occur when a sharp object, such as a nail or splinter, penetrates the skin and underlying tissues. These injuries can lead to localized pain, swelling, and redness at the site of the puncture. In some cases, infection can develop, resulting in increased pain, pus, and fever. The presence of a foreign object may not always be visible, making proper diagnosis important. A podiatrist will typically perform a thorough examination, possibly including X-rays or other imaging tests, to determine the extent of the injury and whether any debris remains embedded. Timely treatment is essential to prevent complications. If you have sustained a puncture wound on your foot, it is suggested that you consult a podiatrist who can successfully treat this condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Scott Shrem from Garden State Foot & Ankle Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Hazlet, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018









